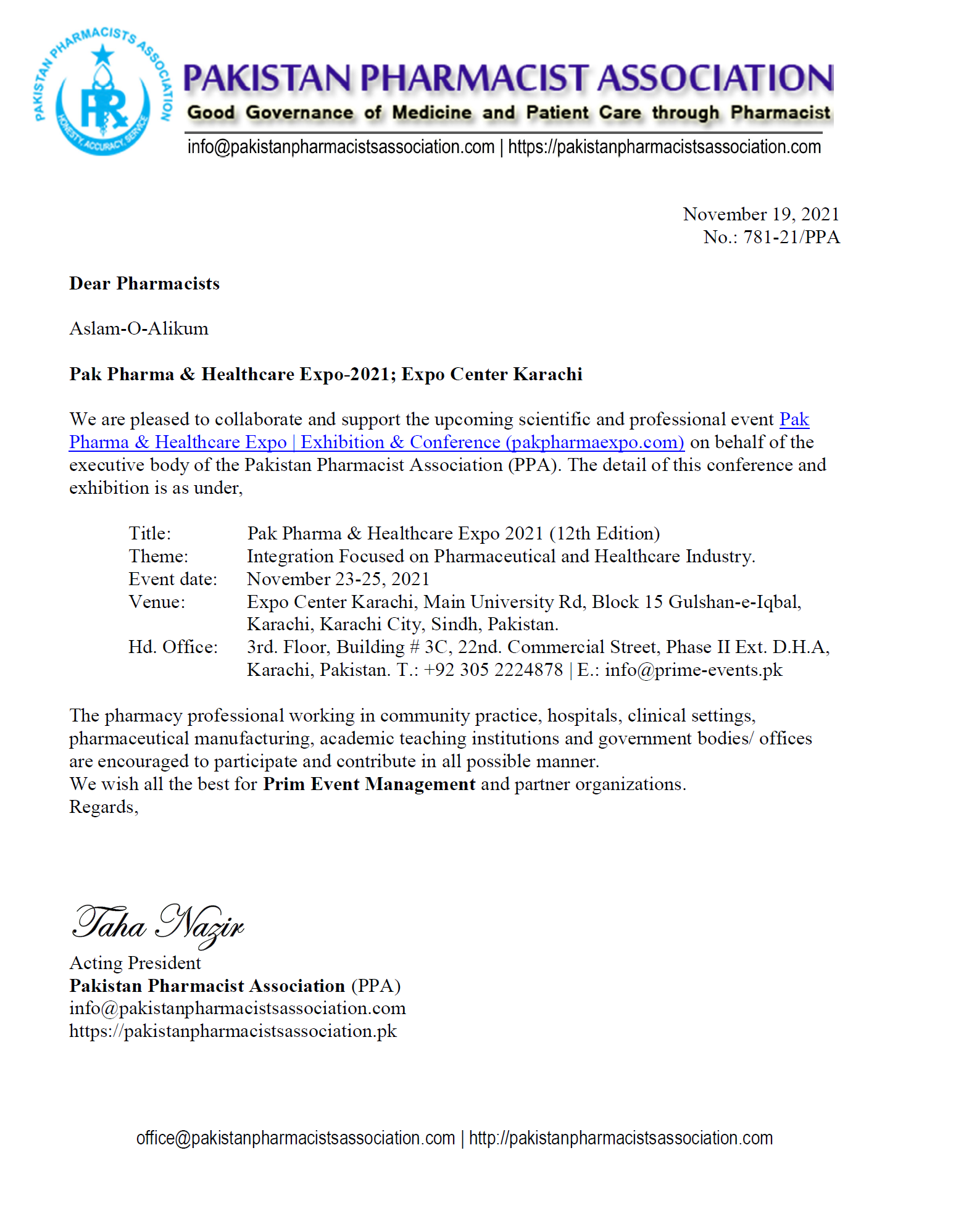
Stafff Reporter (Pharmaceutical Review). Iffat Ullah Aziz Chief Election Commission of Pharmacist Federation (Pakistan) C.: +92 317 0744544 has completed the electoral procedure of Pharmacist Federation (Pakistan) session 2021-22. He has notified that Executive Members have cast vote as described in Sub-section-III; clause 11-36 of the constitution of Pharmacist Federation (Pakistan). Malik Iradat Hussain (+92 300 5016346) has received majority and elected as president for aforesaid session.